Review: GLP -1 & Diabetes
*Disclaimer : Speak to your healthcare provider before making any changes to your medication regime. This blog is the experience of 2 people living with diabetes & using GLP-1s.
One of the hottest debated topics in the world of diabetes today is the use of GLP-1 medications to manage blood glucose levels and even weight. Better known as Ozempic, Mounjaro, or Semaglutide, these GLP-1 agonists have been in the news for celebrity usage and quick weight loss in non-diabetics.
Some celebrate them as game-changers, others caution against overuse & many prefer to stay silent but whether you welcome or worry about GLP-1s, their impact on diabetes & health conversations today is impossible to ignore.


Pictures of Serena Williams & Karan Johar from the internet
But how does it work? Is it really beneficial for people living with all kinds of diabetes? And should you consider it?
This blog post will break down the basics of GLP-1 agonists, real experiences, and more.
What is GLP-1?
GLP-1, short for glucagon-like peptide-1, is a natural hormone your body makes in the gut after you eat. Its job is pretty clever; it tells your pancreas to release insulin when blood sugar rises, slows down how quickly food leaves your stomach, and even signals your brain to feel fuller sooner.
Together, these actions help keep blood sugar steady and reduce overeating.
Scientists have created medicines that copy the effects of this hormone, known as GLP-1 receptor agonists. One of the most effective is semaglutide, a drug designed to act like GLP-1 but last much longer in the body than the hormone itself.

If you’ve heard of Ozempic, that’s actually just the brand name for semaglutide when it’s prescribed to people with type 2 diabetes. Ozempic helps lower blood sugar, reduces the risk of certain heart problems, and often brings the added benefit of weight loss.
Snehal's Experience
As someone living with type 1 diabetes for the past 23 years, my insulin needs, appetite, and weight have always been a juggling act. My HbA1c has usually stayed between 6.2 and 7, which is considered excellent control.
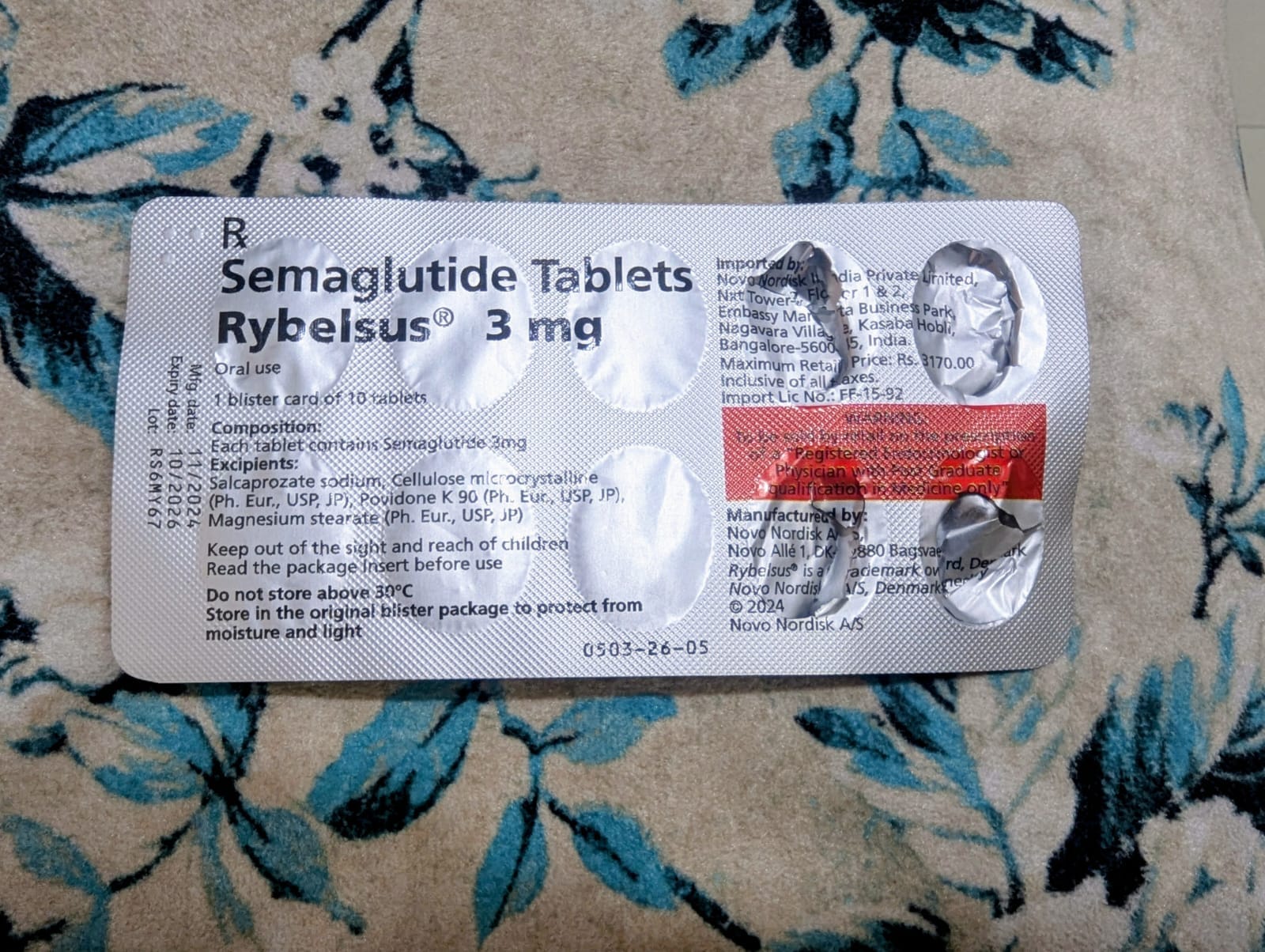
This year, during my annual routine tests (read more about routine tests here) I noticed my cholesterol had shot up and I’d started seeing signs of frozen shoulder. I was also 89 kg—overweight for me. My doctor suggested Rybelsus (oral semaglutide) to help with weight management, which in turn would help reduce cholesterol. I started taking a 3 mg dose in April 2025.
Within two weeks, my appetite had dropped almost by half. My daily insulin doses came down too, but at first it was a nightmare to adjust. I wasn’t sure how much I would eat or how much insulin to inject. I tried my “sick day” logic (read the sick day management protocol here)—reduce by 2-4 units and ended up with severe hypos all day (read our hypo guide here). It was draining to say the least. After a lot of trial and error, I figured out what worked for me. My daily insulin requirement eventually reduced by about 35–40 %.
The weight loss was dramatic—from 89kg to 84kg in 2 weeks. But it wasn’t a smooth ride.
I began to feel uneasy in my stomach—queasiness at the thought of food, burps, and a constant nauseous feeling throughout the day. A few sips of Diet Pepsi after meals seemed to calm it. I also tried some home remedies to soothe my tummy, which didn't help much.
By the fourth week, I also started puking a little bile (also called “pitt” in Marathi) in the mornings while brushing my teeth. Some days I skipped my dose because my stomach felt off.
Then came a scary incident. I had an early morning flight (which meant less sleep and travel stress), and things spiraled. I vomited bile at the airport and continued puking throughout the flight. I had skipped Rybelsus that day, but the impact showed. I kept feeling uneasy throughout my trip and couldn't eat anything. I stuck to what felt like comfort food at that point—lemon juice, lots of cucumber, and simple rice dishes like dal chawal or khichdi.
I updated my doctor about my situation, and they advised me to stop Rybelsus for a while; avoid tea, coffee, fizzy drinks, alcohol, and take antacid medication twice a day.
We also decided that it's best I stop Rybelsus a day before travel. I took a break for almost a month after this experience. Do note that the effect of Rybelsus lasts for several weeks even after you stop taking it. When I had to travel early again, the pattern repeated even though I’d stopped Rybelsus the day before. After that, I’ve stopped Rybelsus completely and am waiting to discuss next steps with my doctor.
In 4-5 months, with breaks in between, I lost about 10 kg. I’ve continued to work out 3-4 times a week, and food intake was minimal because of Rybelsus.
Here’s what I’ve figured out so far :
- I was on the 3 mg dose the whole time. I journaled my experience, taking notes of when I had issues and how my body felt. This helped me have better discussions with my doctor.
- Rybelsus definitely suppressed my appetite and helped me lose weight.
- It also slowed my stomach emptying; after restarting after a break, I began noticing late post-meal glucose spikes on my CGM, 3-4 hours after eating. Read our blogs on diabetes tech in India here and see the video playlist here.
- Travelling, lack of sleep, stress, and Rybelsus don't work well for me. They made the nausea/bile episodes worse. I now stop Rybelsus a day before travel to reduce the chance of an episode. Read our blogs on travel & diabetes here and see the video playlist here.
- My alcohol intake has been minimal, but with Rybelsus, I didn't feel like having much alcohol—now just the occasional glass of wine. Surprisingly, I didn't feel like having coffee either, even though I love my Americanos.
- The pill is to be taken on an empty stomach first thing in the morning. Recommended wait time before eating anything is 30 mins, but I feel uneasy at 20 mins, so I eat something light like a cucumber or a moong-besan chilla after 15-20 mins. (As discussed with my doctor). PS- did you know you can look up the macros of any food either on the Blue Circle Diabetes app or this link.
- You may also feel constipated as your food intake drastically reduces. Staying hydrated helps. I usually drink 4+ litres of water daily and continue to do so.
- Rapid weight loss can bring its own issues like hair shedding or nutrient deficiencies, so make sure you’re getting enough protein, iron, and micronutrients.
Everyone’s experience with GLP-1 drugs is different. Many people I’ve spoken to manage the mild nausea with simple home remedies. For me, the side effects were intense enough to need breaks and medical advice.
If you have a history of bloating, burping, or acid reflux, or live with type 1 diabetes like me, keep a close eye on your blood sugars and stomach symptoms.
Work with your doctor, start low and slow, keep a symptom diary, and don’t ignore severe nausea or bile vomiting. Sometimes breaks help your gut recover; sometimes a different approach or dose is needed.
I’m still figuring out what balance works for me. Rybelsus has been a powerful tool, but not an easy one. My hope in sharing this is to give a real-life glimpse of both the benefits and the bumps along the way.
Please remember: Rybelsus, like other GLP-1 drugs, can have additional side effects—including risks such as worsening diabetic retinopathy. Always read the patient information leaflet that comes with your medication and discuss any concerns with your doctor.
Nishtha's Experience
I live with type 1.5 diabetes and deal with strong insulin resistance as part of my condition. Once I began with insulin therapy—and Metformin continuing—I rapidly put on weight and gained over 30 kgs in four or so years. It became a vicious cycle—I'd put on weight, would have to increase my insulin dosage, which would make losing weight harder. Despite my 5'8" frame, nearly 90 kgs was a problem figure.
No amount of gymming, home exercises, swimming, or beyond would move the needle on my weighing machine. I could live with the weight gain, but it brought along with it the increase in insulin my body needed, as well as the risk of heart disease. That wasn't acceptable to me.
While looking into ways to circumvent this issue, I read up more about "Ozempic". At this point, it was already being touted as the weight loss drug Hollywood swears by, but on reading further, I realised it was meant to be used in treatments for type 2 diabetes. More importantly, I read about the effect it had on the ability to control HbA1c levels and decided to ask my doctor about it. While it's not typically used for insulin-dependent diabetics, doctors can prescribe it to you in case of insulin resistance.
While Ozempic wasn't officially available in India just yet, my doctor informed me Rybelsus, a semaglutide, had been available for close to a decade here. With her blessings, I began using it.
You're expected to be on a 3 mg dose for the first month—also called the wash-in period. A smaller dose helps your body acclimate to the drug better, and the side effects are relatively less intense.
I did deal with acidity, constipation, and severe loss of appetite around the first month. But it was to be expected. The following month—especially after having trained myself to eat better and from time to time—I moved my dose up to 7 mg. A couple of months of this, and I started seeing a marked improvement in blood glucose stability and saw my weight drop.
Next, I moved on to a 14 mg dose after four or so months, and saw my weight go even more rapidly. However, it also suppressed my appetite a lot more and caused several hypoglycemia events. With every change in dosage, I'd have to go back to the drawing board and reassess my diet plans, my basal dosages, and exercise regimen.
Finally, having hit my weight goal of 70kgs—and with worsening hypo symptoms—I spoke to my doctor about dropping back to the 7 mg dose. The idea was now to maintain a plateaued glucose range as well as a weight range.
Over the course of a whole calendar year of going from Rybelsus 3 mg to 7 mg, to 14 mg, and now back to 7 mg, my HbA1c levels dropped from 7.4 to 6.2. Now ranging between 6.6 and 7, my weight stays between 65—70 kgs. A surprising upside to all of this has been that my sleep quality has drastically improved, with deeper sleep for longer being more common now.

Here are some tips I've picked up along the way:
- Keep your medicine strip next to your bed. Have it the first thing on waking up. Do not eat for the next 30 minutes.
- Never miss your dose. If you do, consult your doctor on how to fix the miss.
- Use natural remedies like fennel extract water to soothe your stomach in case of bad acidity.
- Immediately consult your doctor if you feel your acidity symptoms worsening or see side effects not listed in the accompanying leaflet. Always read the leaflet before you begin and if you change your dosage.
- Like Snehal mentioned in her experience, add enough nutrient supplements to your diet. Try to add a fiber supplement and meet your protein goals as much as possible.
- Simply being on semaglutide doesn't mean you can eat what you like. I noticed that excessively rich or oily food would actually make my acidity worse. Stick to your diet not just for the best results, but also to keep acidity symptoms from ruining your day.
- Trust your gut—literally in some cases, too, here. But if you feel like this may not be the solution for you, or if you wish to change your doses, speak to your doctor.
- Do not go overboard with alcohol on semaglutide. Both elements in your body together can reduce your blood glucose levels. Worse, alcohol can irritate your stomach lining. Add to it semaglutide slowing down food digestion, and it makes for a crazy combination. If you have a drink on the regular, you may see a difference in your tolerance levels. We understand navigating alcohol with diabetes can be difficult, see this workshop on the experiences shared by our community. Note- this is not a recommendation to consume alcohol & the video is about sharing experiences, not providing medical advice.
- Drink a lot of water!
Looking back, I don’t see Rybelsus as the thing that "fixed" me, but as something that finally gave me a fighting chance to take charge again. By being able to maintain my blood glucose levels and ensuring my weight wasn't contributing to an increase in insulin dosage, I feel my energy is back.
It’s still a work in progress, but one I feel more in control of now.
Pricing
In India, a strip of 10 tablets of Rybelsus 3 mg costs INR 3,170. For the higher strengths, a strip of 7 mg costs INR 3,520, and a strip of 14 mg costs INR 3,870. Prices vary widely by pharmacy, city, and available discounts, both online and offline—always check current rates locally. At these rates, GLP-1s remain prohibitively expensive for most people living with diabetes in India.
Everyone who needs these medicines should be able to access and afford them, regardless of where they live or their financial situation. Our community, Blue Circle Diabetes Foundation along with several others across the globe have been advocating for the inclusion of rapid acting analogue insulins & GLP-1s to the WHO Essential Medicine List to make them more accessible & affordable for whoever needs them. To that end, we delivered a formal statement at the WHO Open Session of the 25th EML Expert Committee on behalf of a coalition of Indian diabetes organisations, in May this year.

By September, the WHO added rapid-acting insulin analogues & GLP-1 receptor agonists to the Essential Medicines List — a historic win for people with diabetes. Read some media coverage about this inclusion in the WHO EML here and here.

Newspaper coverage about the inclusion in the WHO EML
FAQs
1. Can people with type 1 diabetes take semaglutide?
Semaglutide isn’t approved for type 1 diabetes, but some doctors may prescribe it off-label for weight or insulin-resistance issues. Always do this under medical supervision, as insulin dosing needs can change quickly.
2. How long does it take to notice results?
Many people see appetite changes within a week or two. Blood sugar improvements and weight loss usually become clearer after a few months.
3. What are the most common side effects?
Nausea, bloating, constipation, and sometimes vomiting. These usually ease as your body adjusts, but ongoing or severe symptoms should be discussed with your doctor.
4. Can I drink alcohol while on semaglutide?
Light drinking is usually fine, but alcohol can worsen nausea and increase the risk of low blood sugar (especially if you use insulin). Tolerance may also feel lower.
5. Is semaglutide a long-term treatment?
Yes—most people need to stay on it to maintain benefits. Stopping often leads to weight regain and higher blood sugars, though the exact plan depends on your health goals.
SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetes community. Every little bit helps us in sustaining this endeavour. Our NGO is registered under Section 80G of the Income Tax Act, India.
Click here to donate